Elementary school personal hygiene classes teach us to cover our mouth when we sneeze or cough and keep away from others (except the doctor) if we feel feverish. In reality though, how many of us still practise this diligently; and more importantly, how can we be certain the person next to us is not unwell?
[blockquote text=”The aviation industry needs a prudent and sustainable way to keep unwell passengers apart from others – to combat against COVID-19 and beyond.” text_color=”#004361″ show_quote_icon=”yes”][vc_separator type=’transparent’ position=’center’ color=” thickness=’5′ up=” down=”]
This is the issue we need to address and why the transmission of highly communicable diseases is of such importance for public health control throughout our modern, interconnected world. So why is it that, amongst these highly communicable diseases, Ebola (50%-90% mortality rate) and seasonal influenza (<1% mortality rate), pose less risks than SARS (9.6%), MERS (34.3%) or COVID-19 (1%-3%)?
The majority of Ebola patients become so ill that they are often unable to stand, much less travel to infect others; whereas people infected with seasonal influenza can generally travel and infect others, but relatively few become severely ill. This is where moderately virulent diseases such as COVID-19 are the most difficult to control as they balance between communicability and virulence.
Because these recent coronavirus cases are such unprecedented events, only a handful of airports, during significant epidemics such as 2003 SARS, 2012 MERS and 2020 COVID-19, have ever attempted separating unwell individuals from other passengers.
Passenger health screening: a choice between efficiency and effectiveness
Passenger health screening is nothing novel to the aviation industry. In the early days of aviation, mandatory proof of immunisation records was required during check-in. Following the SARS epidemic, arrival temperature screening was introduced at some airports. The need for this type of screening however, has been infrequent at best; until the COVID-19 global pandemic which has impacted the world at a similar scale to the Spanish Flu of 1918, when air travel was much less common.
There are currently only three forms of health screenings available to identify potential COVID-19 carriers. Even in medical institutions, these have varying level of effectiveness and efficiency:
| Screening method | Determining factor | Process(es) required | Estimated accuracy of ‘one-time’ screening | |
| 1. | Oral/nasal swapping | Viral particles/ components | 1-to-1 sample extraction by medical professional; samples process through laboratory-grade Polymerase Chain Reaction (PCR) machine and batch testing – top grade laboratory (assume lab to be co-located with sampling site) process up to 300 samples (max capacity of a high-end PCR machine) per batch in 2.5-4.5 hours | 80%-95% |
| 2. | Blood sampling | Human antibodies | 1-to-1 blood sampling to be obtained by medical professional; samples concurrently apply on individual rapid test kits for results – about 15 min/pax | 60%-80% |
| 3. | Temperature Screening | Fever | 1-to-1 temperature taking – approximately 10-15 secs/pax | 60%-70% |
| Mass temperature screening – discreet and un-interruptive | 50%-60% |
CAPEX vs OPEX: a sustainable measure beyond COVID-19
Scientists have long debated the effectiveness of temperature screening at airports, but studies so far have been predominately based on data from ‘one-time’ temperature screening of arrival passengers requiring CAPEX investment on temperature screening devices at destination airports.
Undeniably, oral/nasal swapping and blood sampling represent more effective screening measures for COVID-19 carriers compared to ‘one-time’ temperature screening. The OPEX associated with clinical grade consumables and pool of medical professionals are, however, expenditures that maybe unsustainable for the aviation industry. In the long run, the expense would be passed on to passengers in the form of levies/surcharges.
It is considered highly probable that SARS-CoV-2 (the virus that caused COVID-19) will mutate into a different strain. Preliminary studies have revealed three variants of SARS-CoV-2. Unlike temperature screening, rapid test kits and mucus testing procedures are specific to each strain of virus. New kits and procedures would be required if a new virus (or a mutated SARS-CoV-2) emerged as another global pandemic threat.
Temperature screening in the medical sector
Rudimentary as it may sound, taking a patient’s temperature remains one of the most widely used form of medical assessments in clinics, medical centres and hospitals. While generic in nature, it is a rapid and straightforward indicator of infection response in the human body.
Although a medical doctor will never diagnose your condition simply based on your elevated body temperature, it provides strong evidence of someone being physically ill – from COVID-19 or just a common cold. If information is available, would you like to be walking, queuing, or sitting next to someone who is clearly feverish?
There are currently no single screening procedures that can immediately and confidently identify COVID-19 patients, even in hospitals. The imperfect nature of biomedical tests means that even mucus/blood tests have to be administered repeatedly to achieve statistical confidence. For medical professionals responding to physically unwell patients, the best option has been, and will continue to be: warding, multiple testing and continuous (including body temperature) observations.
The aviation industry can conduct continuous temperature screenings throughout a passenger’s journey
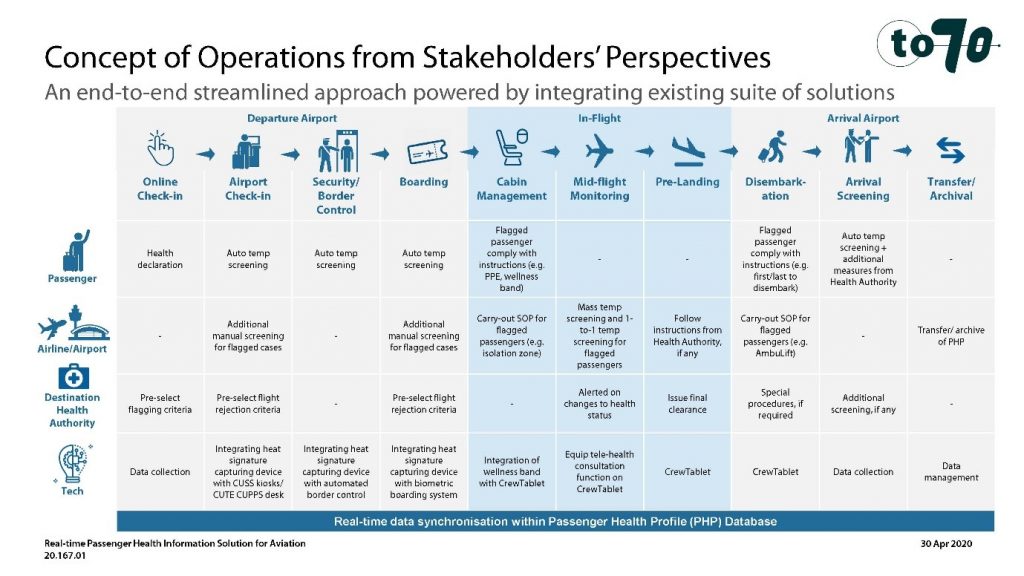
Our industry can take a lead in enabling passengers travel by establishing protocols that allow unwell passengers to be identified and either turned-away (before flight) or isolated (unwellness developed in-flight). Technology and procedures are available now. From check-in to arrival, multiple temperature screenings can be performed at existing passenger touch-points in an end-to-end, streamlined approach.
Temperature screenings throughout the entire passenger’s journey in a layered approach can deliver high levels of confidence that unwell passengers are identified and appropriately managed. In addition, multiple screenings from check-in to arrival can attempts by passengers to deliberately suppress fever symptoms through consumption of antipyretic agents.
When complemented with targeted screening measures on high-risk, ‘flagged’ passengers (by public health authorities) due to travel history and risk-based criteria, continuous temperature screening can be an effective, robust and sustainable approach to boosting passenger confidence in air travel. As an air passenger, you will be assured that fellow passengers on the same 12 hours journey as you, are not fighting a potentially communicable infection.
While asymptomatic carriers may be missed by temperature screening (in fact even with mucus/blood tests), this may be equivalent to the risk we will be exposed to in our own society with governments relaxing restrictions gradually. Unwell citizens have been urged to stay at home and immediately seek medical help without interacting with others. But what if the train passenger next to you appears perfectly healthy yet he/she is an asymptomatic carrier? Travelling by air, at least you know that all passengers’ temperature are being continuously monitored throughout their journey.
About To70. To70 is one of the world’s leading aviation consultancies, founded in the Netherlands with offices in Europe, Australia, Asia, and Latin America. The environment has been part of our DNA. Since its inception in 2000 To70 has played a leading role in the efforts to reduce environmental impacts of aviation. With our thorough understanding of these impacts, airspace management, air traffic operations, safety and aviation policy, we are capable in developing practical and feasible solutions for a quieter and greener aviation. For more information, please refer to www.to70.com.